Breast Reconstruction: Finding the Right Fit for You

A new diagnosis of breast cancer can be a very emotionally overwhelming and taxing time for a woman.
When you are in the care of a breast cancer certified center of excellence, like at NMHS, you can be sure your diagnosis, treatment and reconstruction go as smoothly as possible.
As a member of the American Society of Plastic Surgeons and a board-certified plastic surgeon at North Mississippi Medical Center, I work very closely with our Cancer Care team to make sure everyone who desires or is curious about reconstruction has the opportunity to learn about the options and achieve your goals.
The process and treatment options for breast reconstruction are constantly changing and improving. I do my best, along with our breast surgeons, to make sure every patient has access to the most up-to-date techniques available. There are many different surgical options and timelines available – there is no single option that is right for every patient.
When I speak to my patients about reconstruction, I first try to explain the options in three parts:
- The timeline – when reconstruction begins
- Immediate: starting reconstruction on the same day as the mastectomy
- Delayed: starting reconstruction months or years after the mastectomy
- The mastectomy technique – depends on your breast surgeon, cancer location and body type
- Traditional: a horizontal incision that removes the most skin with breast tissue
- Skin sparing: an incision similar to what is used in breast lift or reduction surgery that saves as much of the skin as possible
- Nipple sparing: an incision below the crease of the breast that saves the skin as well as the nipple
- The reconstruction technique
- Autologous: using a woman’s own tissue
- Implant-based: using a combination of tissue expanders and implants
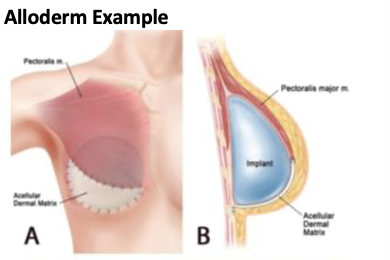
When patients choose to have immediate reconstruction, we begin their reconstructive journey on the same day as their mastectomy. This process involves coordinating with the breast surgeon who removes the breast tissue and then a plastic surgeon who places tissue expanders. In my practice, I generally place the tissue expanders under the chest muscle and support it from the bottom with a sling. This allows patients to save one operation and minimize their time without breasts. New mastectomy techniques, like spy angiography – which can check the safety and blood flow in their remaining skin – and new reconstruction materials have made this possible. This immediate tissue expander-based reconstruction has quickly become the standard of care.
Another advantage to performing immediate breast reconstruction is that it allows us to save more of the skin or even the nipple to allow for the most natural breast reconstruction possible. For these patients, I attempt to use similar incisions for those patients undergoing breast lifts or breast procedures which are more easily hidden and cosmetically appealing.

However, even when beginning on the day of the mastectomy, the timeline of reconstruction is not short. Even in those patients who choose to have immediate reconstruction, the healing process involves beginning to fill the tissue expander placed during the initial operation around two weeks after the surgery. We typically add fluid weekly until we reach the desired volume – most patients can achieve an appropriate size around four to six weeks after the operation. If the patient does not need radiation, we can proceed with the second surgery in their reconstruction around three or four months after the first procedure. This surgery is much simpler, and patients can go home the same day. During this surgery, the tissue expander will be replaced with a much softer, more natural gel implant. Often during this operation, we will also perform fat grafting to transfer excess fat from the abdomen to the breast to provide more coverage over the implants and achieve a more natural result.
After the second operation, patients who choose to pursue nipple reconstruction can have these procedures done, usually under local anesthesia only. Tattooing can be used to optimize or as an alternative to surgical techniques by a licensed professional. Depending on a patient’s anatomy and preferences, some are candidates for nipple-sparing reconstruction, where the nipple is left in place during the initial operation, or nipple reconstruction with free nipple grafts. These techniques allow us to save as much tissue as possible.
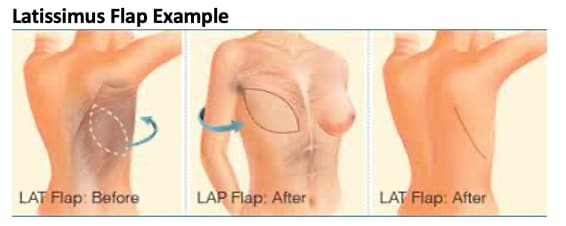
Patients who choose to treat their cancer but pursue reconstruction at a later time fall into the “delayed reconstruction” category. While more traditional, this pathway is sometimes appropriate for patients who wish to address their cancer treatment and reconstruction separately. For these patients and most patients who have had radiation, I recommend performing reconstruction using skin from the back with a tissue expander. This tissue from the back can be used to provide healthy skin, muscle and fat over a tissue expander to replace what was lost during the mastectomy. This is also a salvage technique for patients that may have had complications during attempts at immediate breast reconstruction.
No timeline or procedure is perfect for every patient, and during my initial consults with patients with breast cancer, I listen to their personal goals and cosmetic preferences when deciding what works best for them.
If you choose to have reconstruction after a mastectomy, you have options to choose from based on your diagnosis, your treatment plan and your personal preferences.